
The Mobi-C Cervical Disc is an artificial cervical disc implant composed of three pieces: two end plates and a plastic insert.
The Mobi-C Cervical Disc is the global leader in cervical disc arthroplasty.1 Since 2004, over 225,000 Mobi-C Discs have been implanted across 26 countries.
Mobi-C Cervical Disc was the first cervical disc in the U.S. approved to treat more than one level of the cervical spine, and Mobi-C is a proven cervical disc with 10-years of clinical data showing improved long-term outcomes for one- and two-level replacements.
At 10 years, all patient-reported outcomes of Mobi-C recipients were equivalent to or improved from 7 years. Recipients of Mobi-C reported improved Neck Disability Index (NDI) Scores, improved neck pain, and improved arm pain. In addition, no subsequent surgery at an adjacent level occurred between the 7-year and 10-year follow up.2,3
History
Mobi-C was designed by a team of experienced French surgeons and was first implanted in France in November 2004. in 2006, Mobi-C entered into FDA IDE one- and two-level studies. In August 2013, the FDA approved Mobi-C for use in the United States, making Mobi-C the first cervical disc FDA approved to treat one- and two- levels of the cervical spine. The FDA also determined Mobi-C to be statistically superior to fusion at 7 years for 2-level cervical disc replacement.2,3
A return to physiological mobility
The controlled mobility of the patented adaptive core is the foundation of Mobi-C. With vertebrae and neck muscle movement, the Mobi-C implant is free to twist and slide left-to-right and front-to-back, as well as rotate. This allows the vertebrae above and below the Mobi-C to move. This feature is designed to allow the disc to self-adjust and move with the spine, which is intended to facilitate motion similar to the natural cervical spine.
A bone sparing cervical disc option
Mobi-C is a bone sparing cervical disc option. With Mobi-C, there are no invasive keels or screws required for implantation. The lack of invasive keels and screws eliminates the need for bone chiseling and preserves the vertebrae for a stable surface ideal for one or two-level implantation.
Rather than screws or keels, the Mobi-C plates have teeth on the top and bottom that help hold the plates to the vertebrae. The teeth are pressed into the bone with no bone cut out, which makes the Mobi-C design and technique bone sparing
Materials
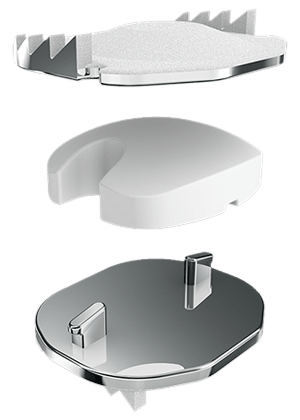
The Mobi-C disc has three parts: two metal plates and a plastic insert in the middle. The plates are made of a mix of metals commonly used in spine surgery (Cobalt-Chromium
Molybdenum Alloy).
The outside of the metal plates are sprayed with a coating (Plasma Sprayed Titanium and Hydroxyapatite). This coating helps the vertebrae to grow and attach to the metal plates for long term stability.
The plastic insert is made from Ultra-High Molecular Weight Polyethylene. The insert is flat on the bottom and round on the top. The insert is made to move as you move your neck.